Hospitalogists,
I’ve been talking with an innovative company looking to redefine healthcare, and I’m excited to share this essay with you guys today.
PEP Health is that company, and what their team is building for payors & risk-bearing organizations could make a significant impact on the future of care delivery.
At its core, PEP Health is solving a simple, yet notoriously complex, problem in healthcare.
What is quality?
So today, we’re going to dive into PEP Health’s story and why it’s one you should pay attention to – especially if you’re a payor or risk-bearing organization trying to understand how patient experience ties into quality scores and shortcomings of your network.
This is a sponsored deep dive in partnership with PEP Health. I write these from time to time with companies I personally believe are doing interesting work in various areas of healthcare like patient experience and value-based care. If you’re interested in partnering with me on a sponsored deep dive, where I tell your story in my voice, feel free to reach out at [email protected]!
PEP Health Key Takeaways
PEP Health is a patient experience and user feedback platform.
With its AI-enabled patient experience dashboard, PEP has analyzed over 35 million public patient comments across review sites and social media along with 8.5 million URLs.
By doing so, PEP provides actionable insights to payors and providers, helping them understand how their patients are receiving care, their perceived care experiences, & feedback from those encounters with their networks.
In general, the ability to differentiate on quality – or compare quality across plans or providers – is difficult today.
With its proprietary ‘PEP’ Score, PEP Health is redefining what quality actually is and giving the patient a voice at scale – where perhaps someday in the near future, they can differentiate MA plans based on quality and not just price.
PEP Health can tell people where care is good and bad, and why – and compare that against anything you’re interested in across the U.S.
Patient experience measures are a major factor in Medicare Advantage Star ratings calculations. The patient experience is tied closer to reimbursement than ever before and this dynamic will continue to grow.
PEP Health improves Star ratings (AKA, increases payor revenues) through better, real-time insights into patient experience.
To learn more about PEP Health’s platform, get in touch with their team here!
They’re also going to be at HLTH in October and NGPx in December if you want to meet them there.
Who is PEP Health, and what problem are they solving?
PEP Health founders Dr. Alex Griffiths and Dr. Meghan Leaver crossed paths in a fateful way. As a practicing physician, Alex helped monitor UK healthcare delivery quality across its various departments, but he was dealing with a festering problem.
Scandals, and associated patient abuses were breaking out across the UK. But Alex couldn’t quite understand why – or how. The survey data his team collected from patients were saying everything was fine. How could these terrible incidents keep happening with no indication or warning – not even a yellow flag raising?
It was at this point that Alex and his team found the actual patient chat rooms and online forums.
And you can pretty much guess what patients were saying in these more informal settings versus the formal health inspector survey or report. What Alex found painted a drastically different picture than what had been represented to him for months…even years.
Meanwhile Megan was working on a similar problem – how do we reduce patient harm in healthcare, and could she identify potential causes of harm accurately? Finally, are there tactical, psychologically proven methods to allocate resources in an efficient way to reduce adverse public health events?
Shortly thereafter, the two found each other and realized they were working on similar problems. They published a study together proving that purely by listening to patients in the public domain, you can predict with extreme accuracy what the results of health inspector reports would be 6+ months later.
After realizing what they’d stumbled across and the commercial impact of their solution, Alex and Megan formed PEP Health, expanded into the black box that is U.S. healthcare after the pandemic, and sought to solve an impossible question:
“How do we better define and quantify the patient experience?”
The Patient Experience Quality Problem
The U.S. healthcare industry – despite all of our complaining about consolidation and monopolies – is more competitive than most other countries. And in a perfect world, provider organizations want to acquire patients and keep patients by proving they are delivering great, high quality care.
Meanwhile payors want to acquire members and prove to their customers that they have high quality networks while getting the best bang for their buck (in theory).
This breakdown is a bit reductionist, but it works for our purposes to describe the problem PEP Health aims to solve. What’s the common thread between payors and providers despite the push-pull dynamic?
Quality.
The problem is…quality is hard to define. Just ask any PCP, payor or risk-bearing entity.
A recent study – somewhat sensationalized by media but still directionally correct – concluded that “Value-based contracts contained a mean of 10.24 quality measures” and “Primary care physicians faced a mean of 57.08 quality measures across 7.62 value-based contracts.”
So clearly we’re facing a huge hurdle here when it comes to defining what quality actually means in healthcare. It’s not a standardized definition, it varies greatly by payor or plan (Medicaid vs. Medicare, etc.), and it increases admin costs in the system by introducing complexity and having to track potentially dozens of quality metrics.
While the PEP Health team acknowledges how messy this problem is, they know there’s a better path forward.
Their team is laying the groundwork to define and understand quality in a streamlined manner for payors and providers to help them understand the patient experience, and giving patients a voice.
How PEP Health solves the Quality Problem
We’ve established so far that it’s hard to define quality, and current solutions focused on lagging, costly survey data provide little actionable, real-time value to payors and health systems
Adding to this, patients’ collective voices in too many instances are not being heard well. PEP’s answer to this is simple – we’ve been listening in the wrong places.
Historically many provider organizations or payors sourced patient experience data like this from patient surveys, which are then manually sorted and analyzed for insights.
I’ll just come out and say it: patient survey data is useless, and you’re wasting money by collecting it.
It’s costly, takes months to produce, and it’s hard to make changes or glean timely insights from lagging information. Survey tools don’t offer a deeper level of granularity. Therefore decision making gets hamstrung and care quality doesn’t improve while growth suffers.
PEP Health says we can do better than surveys.
Surveys can’t analyze and sentiment-screen 100,000 comments about one of your flagship hospitals or service lines.
So just as Alex found the online forums and social media posts blasting UK Healthcare clinics, PEP Health developed a dashboard pulling in hundreds of millions of data points from Google, Twitter, WebMD, RateMDs, Vitals, Yelp, HealthGrades, HealthSoul, ZocDoc, patient chat forums and more – patient sentiments, comments, and reviews – across a myriad of patient experience categories with the goal of providing better data than surveys, faster, and in a more efficient manner.
What kind of data is included? These categories include key satisfaction components like fast access to care, transparent billing, or continuity of care and can be seen in the snapshot of PEP’s dashboard below:
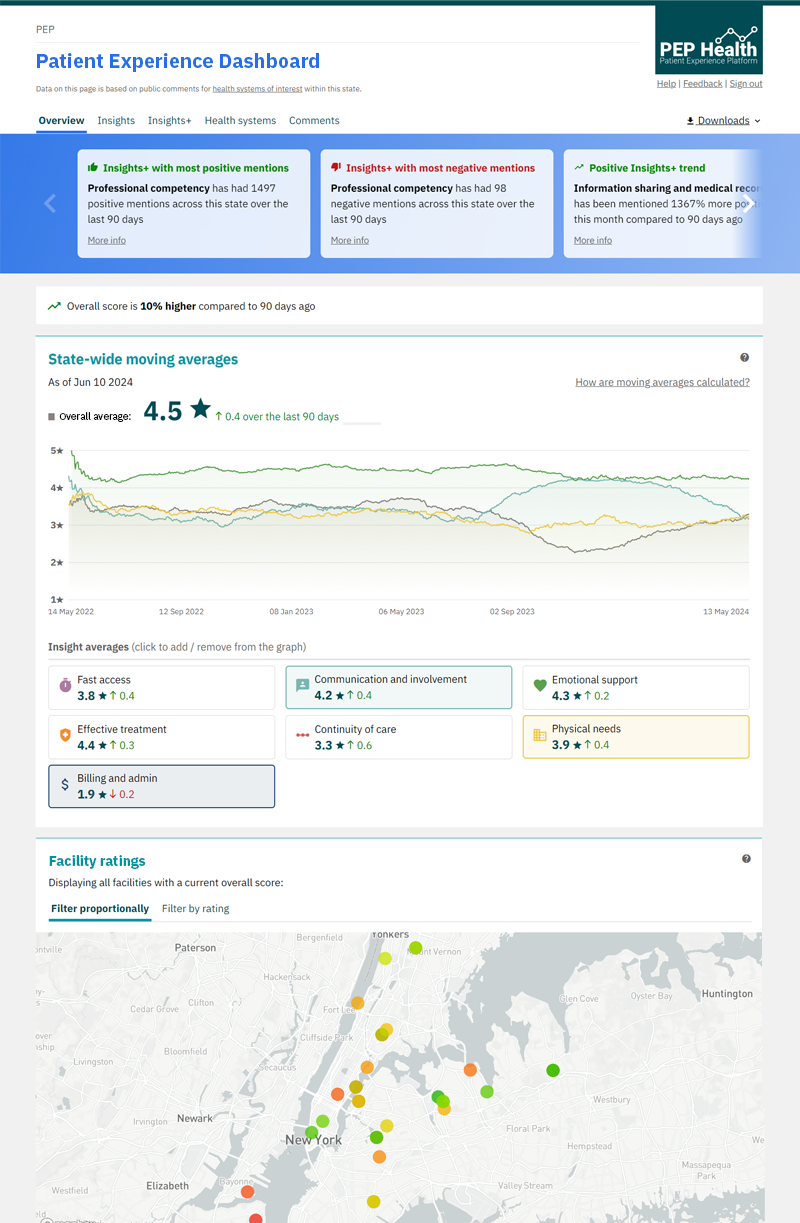
The PEP Health team walked me through a demo of the platform built from the ground-up (and you can watch a walkthrough of their platform here) and explained how most things work. PEP’s dashboard integrates easily into existing technology and provides two outputs: a higher level view of your local market or footprint, and then report-level views that can drill down into key areas of focus.
For instance, if you wanted to look at oncology costs in Florida or orthopedic surgery performance in New Jersey, you have the ability to do so (which provides interesting competitive intelligence opportunities beyond just patient experience metrics but I digress).
On an ongoing basis, PEP’s proprietary AI and machine learning (see – you knew I’d sneak in AI somewhere) algorithms track new comments and crawls across the internet to incorporate new feedback. At this point PEP’s platform tidies up the results and scores the comments or sentiments based on what a patient said.
There is, of course, the ability to review the source data or reviews. PEP’s AI can surface interesting insights like what’s trending up or down, or things mentioned the most – a particular nurse or doctor who often gets called out for good communication, for example.
Now I know what you’re thinking at this point, especially the doctors and clinicians reading this, because I was thinking something similar – “but patients have no idea what they want. How can I know PEP’s data is accurate?”
Case in point:

(Really I just wanted to incorporate that meme in here somehow – maybe one of the best healthcare tweets of all time).
And yes – absolutely – certain patients have idiosyncratic needs, preferences, or requests to drive the most patient physician up a wall on her best day.
But because PEP collects information at a population level with hundreds of millions of data points, these reviews get filtered out. PEP also trains its AI-driven algorithms to collect and summarize the most nascent points of feedback, and also gives you the option to filter by review type or medium on the dashboard. So, if you really want to look at those crazy Florida man patient reviews with your team, have at it (and please tag me on the good ones!)
So in theory, anyone using PEP Health’s platform would hold an accurate, real-time depiction of one of the most heavily weighted categories – patient experience – into Star ratings, AND this person could see which parts of the network might be falling short and causing problems (or outperforming).
PEP Health found that by aggregating the above patient experience factors into a proprietary PEP Score, their team could accurately validate these PEP scores to quality measures leveraged in HEDIS scores, meaning they’re one step closer to a standardized quality score.
In fact, PEP Scores are getting incorporated as a quality KPI into certain contracts with a few of their payor partners in upcoming negotiations.
Why PEP Health is a Game Changer for Payors, Risk-Bearing Entities, and Policymakers
After seeing results from its dashboard and PEP Score, PEP Health has won several customers over the course of 2024 and they hold solid momentum as they continue to scale out the product and add AI-enabled improvements. In several cases, PEP’s clients stopped performing costly surveys altogether given PEP’s relative affordability. Payors and provider organizations giving up paper and faxes…shocking.
What are some other tangible benefits and ROI from partnering with PEP?
As a payor, using PEP’s solution unlocks the potential for significant downstream positive economics:
- Higher satisfaction and better engagement with members leads to better HEDIS scores → higher STAR ratings → more revenue (at a time when MA has hit the fan);
- Deeper understanding of where your network is performing well versus where patients aren’t getting the care they expect; as a result, better network design (especially in narrow networks);
- PEP helps payors understand levers between cost and quality – for instance, you might push on cost too much and see it impact experience;
- Competitive intel and ability to drill down into different MSAs, specific specialties, or any area of focus;
- Potential for more accurate contracting and pricing in value-based care arrangements around experience metrics that matter to patients (Payors can adopt PEP Health’s proprietary PEP Score and tie it to reimbursement or quality metrics);
- Ability to work with health systems to help them understand care delivery shortcomings, improving population health at a market or state level;
- Standardizing quality metrics, resulting in lower administrative costs (maybe eventually? A guy can dream);
- Health inequality – making sure strategic decisions health plans make generate more equality in outcomes or access.
And as a hospital or health system, PEP can help you answer the following organizational questions and provide the following value-adds:
- How are we really doing against competitors in our market from a consumer experience perspective? Are there high quality physicians out there we need to better align with? Are we good at surgery the way we think we’re good at surgery in service lines that matter to us?
- PEP can also ingest a hospital’s internal survey or other patient experience data to get more value out of what PEP is already doing in the public domain. PEP then can bring internal and external insights delivered in one dashboard (and keeping your data within your system, of course)
- Access to this level of granularity and data around key experience or competitive areas leads to more focused conversations and more tactical decision making within provider organizations
- Ability to drill down into various owned facility locations and see how each one ranks on all metrics of patient experience (e.g., fast access or trouble billing); also the ability to search for certain keywords or phrases (e.g., scheduling or staff, emotional intelligence)
- Ability to introduce some friendly competition between service lines and PEP Scores for each facility / service line at the hospital – everyone becomes focused on improving patient experience.
Wrapping up with PEP Health and why you should reach out
In ending this piece, I really hope I drove home the potential for a risk-bearing organization or a hospital to leverage something like PEP and dive into what was previously a healthcare black box in patient experience and quality.
Day by day, patients are becoming more like consumers and healthcare isn’t ready – so how do you respond to that?
PEP Health – and I – want a future where the patient voice is put first, and where that voice matters. Where patient experience for black Americans isn’t 5 times worse. Quality needs to be tied to financial incentives in healthcare, and what PEP is building holds the potential to be a path to get to that future. Good care and patient experience deserves to be rewarded, and vice-versa.
PEP is strongly positioned where healthcare is heading across multiple dimensions: smarter data, real-time dashboarding, experience driven, value and a quality driven future.
Maybe someday we’ll look back and see PEP Scores as one of the key metrics feeding into future quality scores – and the beginning of REALLY implementing value-based care.
So come on this journey with PEP Health with me, and find out what quality actually means in healthcare by scheduling a demo and seeing if their platform is right for your organization.
Resources & Further Reading from the PEP Health team
Payor Dashboard – Interactive Walkthrough: https://app.storylane.io/share/majkbf2q8edw
What Patients Think: Behavioral Health 2024 Report: https://www.pephealth.ai/news/behavioral-health-experience
CEO Mark Lomax interview on Becker’s Healthcare Podcast: https://www.pephealth.ai/news/giving-patients-a-voice
2024 US Hospitals – Oncology Patient Experience Rankings: https://www.pephealth.ai/news/ranking-report-apr-24
2024 US Hospitals – Cardiology Patient Experience Rankings: https://www.pephealth.ai/news/ranking-report-mar-24
2024 US Hospitals – Overall Patient Experience Rankings: https://www.pephealth.ai/news/ranking-report-feb-24
Powering Patient Experience: 2024 White Paper: https://www.pephealth.ai/powering-patient-experience-2024-white-paper
PEP is also going to be at HLTH (Las Vegas) in October and NGPX 2024 (Palm Springs) in December if you’d like to reach out and meet with their team in person.
